Bartonella: The Epidemic You’ve Never Heard Of, Part 1

This is the first installment of a three-part series on Bartonella, bacteria that is being linked to a wide variety of ailments – many of them chronic, and some of them life-threatening. In part one, I’ll talk about what Bartonella is, and its growing recognition as a potentially very serious infectious disease. Part two will cover the wide array of transmission vectors and illnesses associated with the bacteria, and part three will review the current state of the research and recommendations for the future.
Dr. Ed Breitschwerdt is an expert on infectious diseases and a doctor of veterinary medicine. He also finds himself on the front lines of a quiet but growing epidemic. Bartonella is a bacteria most commonly associated with cat scratch disease, which until recently was thought to be a short-lived (or self-limiting, in medical lingo) infection. Bartonella isn’t new – doctors have known about cat scratch disease for almost a century – but it’s only in the past couple of decades that researchers like Breitschwerdt have started to discover exactly how pervasive Bartonella infecton is in animals and people.
“The main problem with determining whether Bartonella is involved with a particular illness has traditionally been the difficulty of culturing the bacteria from patient samples,” Breitschwerdt says. Some of his earliest work was simply dedicated to finding a better way to identify the presence of the bacteria in an animal or human. It’s fairly easy to find evidence of Bartonella in “reservoir hosts,” or the animals that harbor the bacteria: currently, researchers use a combination of serology and PCR (which stands for polymerase chain reaction) to identify Bartonella’s bacterial DNA in samples.
Finding it in potentially infected humans, however, takes a bit more specialized testing. Breitschwerdt had to develop a specialized growth media in order to be able to culture the bacteria in numbers great enough to detect using a standard PCR test.
Once Breitschwerdt and other researchers had the proper tools to look for evidence of the bacteria they found that Bartonella is literally all around us.
“We have found species of Bartonella in mammals ranging from mice to sheep to sea otters to dolphins,” he says. “There are at least 30 different species that we know of right now, and 13 of those have been found to infect human beings.”
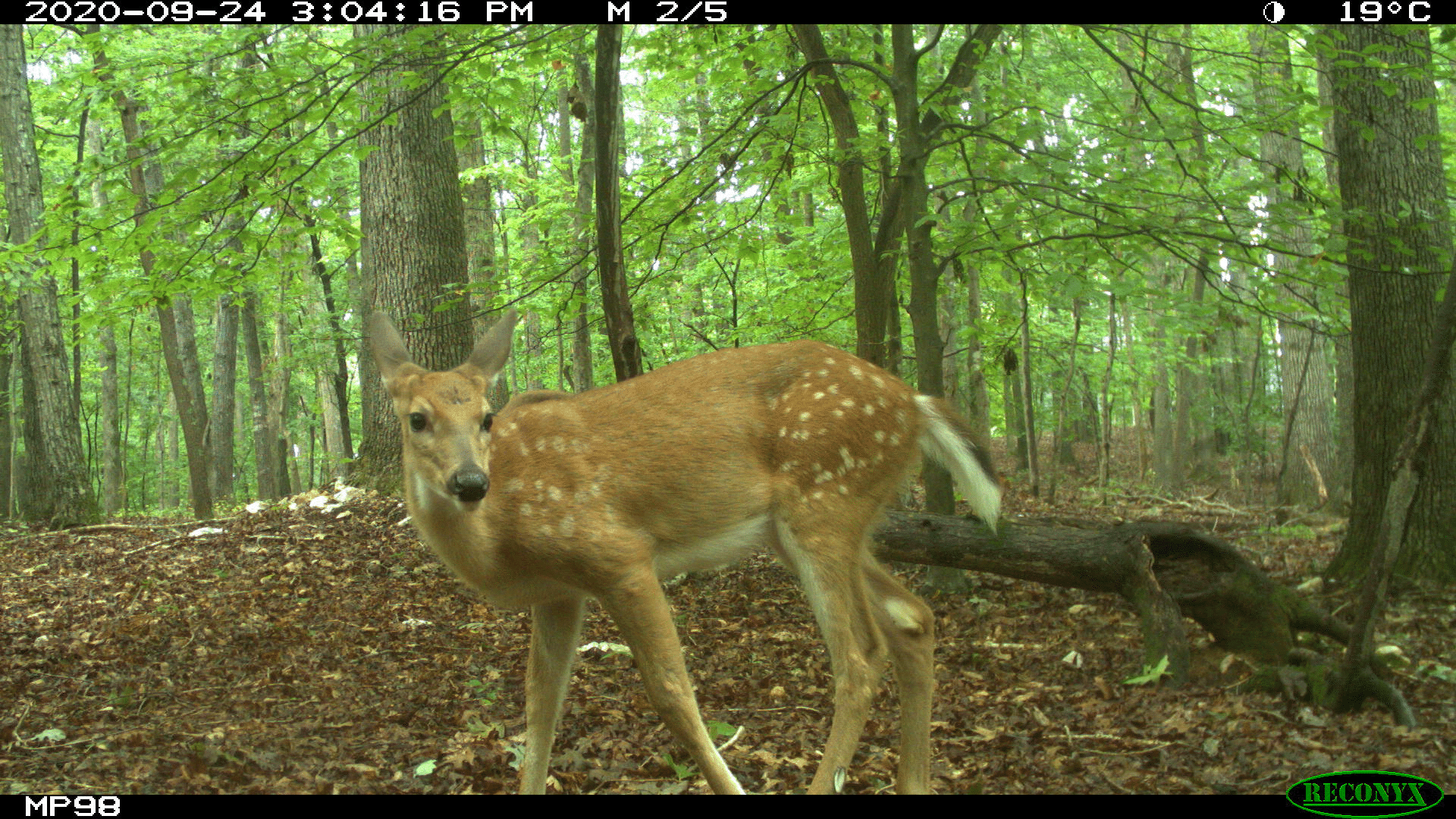
Of course, the likelihood of a human contracting Bartonella from a sea otter is low. But several Bartonella species have found a home much closer to home – in domestic dogs, cats, cows, and rodents which can act as bacterial reservoirs. Fleas, lice – and possibly ticks – also act as repositories for different strains of the bacteria.
Okay, so these bacteria can be found everywhere. People have been getting cat scratch disease for a long time, and it’s usually not that big a deal. What’s changed?
One answer is that our ability to find and diagnose Bartonella infection in animals and humans has led to its identification in patients with a host of “chronic illnesses” that the medical community previously hadn’t been able to attribute to a specific cause. Whether these bacteria cause these chronic illnesses is yet to be determined.
In part two of this series we’ll look at what kinds of illnesses Bartonella is associated with, and who is most at risk of infection.
- Categories: