The rollout of the COVID-19 vaccines has been slower than many people were hoping for. And that has led to various suggestions on ways that governments should modify the plan for getting people vaccinated. The variety of suggestions being put forward can be pretty confusing.
Some are calling for everyone to get just one dose of the vaccine, instead of the two doses used in the clinical trials. Others have proposed sticking with the two doses but delaying the second one until after everyone has received their first dose. Still others are proposing we still give two doses, using the 3-4 week time frame but mix-and-match the first and second vaccines – giving people whichever vaccine is available at the time regardless of which vaccine you got first. Even more recently, the chief advisor to Operation Warp Speed suggested possibly cutting the Moderna vaccine doses in half.
But it’s not clear that many of the suggested changes would even address the underlying challenges that are causing vaccination delays in the first place. So what’s going on?
To learn more, we spoke with Matt Koci, a virologist and immunologist whose work focuses on host-microbe interactions in birds. Koci is a professor in NC State’s Prestage Department of Poultry Science.
This post is part of a series of Q&As in which NC State experts address questions about the vaccines on issues ranging from safety to manufacturing to how the vaccines will be distributed.
The Abstract: Why are some people calling for changes to the plan already?
Matt Koci: In a word, speed. We need to get as many people vaccinated as quickly as possible. Both to save lives and to achieve herd immunity*. We do not want to give this virus more time to mutate in a way where the vaccine no longer protects us.
To achieve this, we need to be vaccinating between 0.5% and 1% of the population each day. That’s 1.6 to 3.3 million per day for the U.S. We began vaccinating people in the U.S. in mid-December. And as of January 4, we’ve only vaccinated around 4.5 million people. That’s roughly the same as the number of new COVID-19 cases that have appeared in the U.S. during that same timeframe. In a race between new infections and vaccinations, photo finishes don’t count. We have to do better.
[*Note: There is strong evidence the vaccine prevents severe symptoms of COVID-19, but we do not yet know if the vaccine prevents you from being asymptomatically infected. This means that someone who has taken the vaccine may still be able to transmit the disease to others. Masks, social distancing and handwashing are still encouraged, regardless of whether you’ve been vaccinated. You can learn more here about the possibility that vaccinated people may still be able to transmit COVID-19. This is an ongoing area of research, and we will share new information when it becomes available.]
The changes to the vaccine plan that some are calling for are all focused on ways to vaccinate more people with the limited supply of vaccines that are currently available.
However, the changes that people have proposed don’t address the problems we’re currently experiencing with the vaccine rollout.

Right now, we don’t have people in vaccine clinics sitting around waiting for vaccine to come from the factory. The companies have shipped over three times more vaccine than we’ve used to date. Even if we doubled the vaccine supply tomorrow, we wouldn’t see a significant increase in the number of people getting vaccinated.
In other words, the vaccine companies are making tens of millions of doses. Those doses have been delivered to federal and state officials. But only a fraction of them are getting into people’s arms. The vaccines are hung up in the federal and state governments’ distribution systems. We have to solve that problem first.
When we get closer to the 0.5-1.0% vaccines in arms per day we may start to exceed our supply from companies, but right now it’s hard to know by how much, if at all.
Pfizer-BioNTech and Moderna are each currently providing about four million doses per week. At that rate, they’ll both meet their original obligations of 100 million doses by June 2021. The U.S. has placed additional orders of 100 million doses from both. Additionally, if the Oxford-AstraZeneca vaccine is given its emergency use authorization – which seems likely – then that would mean another 100 million doses immediately available in the U.S., with another 200-300 million to come.
And none of this accounts for the fact that there are still other vaccines in the development pipeline which will likely start adding to our supply in the spring.
In short, while it is good to have contingency plans, I don’t think it’s time to panic and throw the existing multi-dose vaccination plan out the window until we really know whether the supply of vaccines is causing the bottleneck.
TA: What are the risks if we stick with the original plan? And what are the risks if we start changing things?
Koci: The primary downside to sticking with the existing vaccine plan is that it will take more vaccine per person. If vaccine supply is the major roadblock (which, as we discussed above, seems unlikely), that means it’s going to be a slower process. With cases continuing to skyrocket, hospitals around the country starting to ration care, and what seems to be a lack of political or social will to do what is needed to slow the virus spread, the longer it takes to vaccinate, the more people are going to get sick and die. Also, the longer it takes to reach herd immunity, the longer the virus has to mutate – and, at some point, one of those new mutations may help it get around the vaccine.
However, the risks associated with adopting any of the alternative plans is that we only have data showing that these vaccines work when used the way we are currently planning to use them.
We practice evidence-based medicine in the U.S. We shouldn’t be changing courses of action without the data to back it up.
Based on what we know about vaccines, and the immune system in general, there’s almost certainly some flexibility in timing, dosing, etc. But we don’t really know how much flexibility there is. If we assume we can deviate from the plan, and we’re wrong, we could end up with fewer people getting the level of protection they need.
We already don’t know if the protection from the vaccine prevents infection or just disease. If we dial back on how much protection people get there’s an even greater chance that vaccine immunity isn’t high enough to prevent infection. That could lead to more asymptomatically infected people. That gives the virus more places to hide and mutate only to come back later, with a newly developed resistance to the vaccine. In other words, the virus could mutate around the vaccine if we don’t vaccinate people fast enough, but it could also mutate around the vaccine if we don’t give people as much protection as possible.
Part of the rationale for sticking to the original plan is also rooted in the idea that we practice evidence-based medicine in the U.S. We shouldn’t be changing courses of action without the data to back it up. And looking beyond just COVID-19, if any changes we make to the plan end up making the vaccine less effective than we’ve told people it is, that will lead to even more skepticism about vaccines. This could lead to more vaccine hesitancy for other diseases, leading to more outbreaks of preventable diseases for years to come. COVID-19 is the primary issue here, but we can’t lose sight of the big picture either.
TA: Is there any data to support the idea that changing the plan would work?
Koci: Looking at the results from the Pfizer-BioNTech and Moderna vaccine trails, it looks like one dose provided some protection. We just don’t know if that one dose was as good as two, because we only have 3-4 weeks of data (the time between the first and second dose).

TA: What about other vaccines? Historically, how many involve more than one dose?
Koci: Most vaccines used in the U.S. involve patients receiving multiple doses. The one notable exception is the seasonal flu vaccine. However, that vaccine, tends to be much less effective than other vaccines. Much of that difference is likely due to how the influenza virus changes, but I wouldn’t rule out the idea that two doses in one flu season would work better than one. In fact, there are new types of flu vaccines in development, and most of them are being tested using a two-dose approach.
TA: So why do two doses in the first place?
Koci: To answer that question let’s talk a little bit about the ingenious way the immune system works.
Your immune system has the capacity to respond to trillions of different threats. But it can’t be on the lookout for all those different hazards at the same time. If it did, all of the food you ate would just go to powering your immune system, with nothing left over for anything else. When you’re healthy, your immune cells are largely quiet. Like fire fighters and other emergency services workers who are on call in the station house, your immune cells hang out in specific areas in your body waiting to be called into service. When a threat is detected, they spring into action. Different cells have different jobs. Initial responders work to contain the threat, while others develop the ability to hunt down and kill the invader. The first time you’ve encountered a particular threat, this process, from initial detection to killing and removing the threat, typically takes between 7 and 21 days.
As the threat is eliminated, your immune cells power back down and go back to the station. However, some of the hunter-killer cells (T-cell and B-cells) become memory cells. These memory cells form a quick reaction force whose job is to be ready to pounce if that threat comes back. If the same threat does return, the memory cells respond so quickly you probably don’t even know you’ve been infected. The more times those memory cells are asked to reactivate and kick butt, the longer they survive, and the better they get at protecting you from that threat.
This is how the body decides which memory cells, and how many of each memory cell, to keep around. The more you see the same threat, the more important those memory cells are to the body. Diseases you haven’t encountered again for years, or maybe decades, may be deemed unimportant and eventually fade away.
When we vaccinate people we’re trying to mimic this process. We want the immune system to go through that initial response where it develops these hunter-killer cells, without the person actually getting sick. The ultimate goal is to develop good, long-lived memory cells. The best way to ensure we get a good memory response is to mimic getting infected multiple times by giving the vaccine multiple times.
TA: But at least one of the COVID-19 vaccines uses only one dose, right? How does that work?
Koci: Yes. The Johnson & Johnson vaccine is being tested with just one dose. It’s still in Phase III testing so we don’t know how it will stack up against the others. Please don’t take any of this to suggest that I don’t think the J&J, or any single dose vaccine, will work. It could be very effective. I truly hope that it works as well as the Pfizer-BioNTech, Moderna, and Oxford/AstraZeneca vaccines appear to work with two doses. But we have to wait for the data from their clinical trials.
TA: OK, two doses is generally the best way to get the best protection. Does the second dose have to happen at 3-4 weeks? Can we wait longer, so there’s more time to get more people their first dose?
Koci: Based on what we know from other vaccines, and how textbooks describe how the immune system works, it’s easy to speculate that we could probably wait longer. But keep in mind that these other vaccines – the ones that were not developed for COVID-19 – were developed over years, if not decades. When you’re not developing a vaccine during a pandemic, you have the time to test different doses and timing intervals. And while most of the non-COVID vaccines have a longer time interval between the first and second dose, there’s a lot of variability between those vaccines – and we don’t know why. During the testing of these non-COVID vaccines, did everything they try work, but what’s recommended just worked the best? Or did some combinations not work at all? We don’t know. We don’t have the data to make an informed decision.
TA: Some people have proposed giving people two doses, but not worrying about whether people are receiving the same vaccine for both doses. What are the concerns if people get different vaccines for each dose?
Koci: On paper this makes sense, because you’re showing the immune system the thing you want it to make a good memory response to multiple times. However, this only works as long as the components of the virus are the same in both vaccines. And while there is some overlap, the COVID vaccines don’t share all of the same components of the virus.
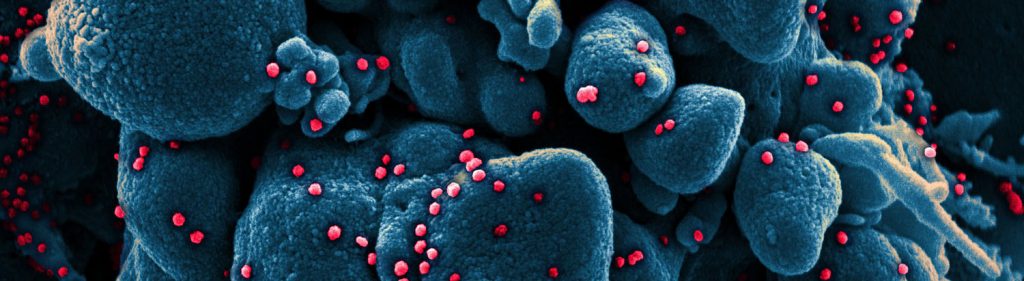
Vaccines deliver the parts and pieces of the virus that we want the immune system to respond to, but they also have other things in them. Chemicals, proteins or other ingredients that protect the main part of the vaccine when it’s injected so it can get to where it needs to go in the body to have the greatest effect. There are thousands, if not millions of cells, representing dozens of different cell types involved in an immune response. Different types of vaccines can lead to different combinations of these cells getting activated. I can’t think of a specific reason why this wouldn’t work, but I also can’t think of a situation were the first and second doses were not only from different companies, but were completely different types of vaccines. The issue here still comes back to we don’t know what we don’t know, and we don’t have data.
TA: What about the proposal that people receive only half the dose of the Moderna vaccine? What’s the idea there?
Koci: So the rationale here is that the Moderna vaccine has over three times the amount of mRNA than the Pfizer-BioNTech vaccine, and the results from the two trials are pretty much identical. So the thinking is: maybe we don’t need all that “extra” mRNA in the Moderna vaccine; if we gave people half doses they would still get more mRNA than in the Pfizer-BioNTech vaccine, and we could double the amount of available doses.
The issue here is the Moderna vaccine also doesn’t have to be kept as cold as the Pfizer-BioNTech vaccine. We know mRNA degrades quickly and so needs to be kept as cold as possible. I don’t know, but maybe the reason Moderna’s vaccine still works, despite being stored at -20 degrees Celsius instead of -80 degrees, is because they’ve added more mRNA to account for the loss at the warmer temperature. If we start cutting doses in half, people may not get as much functional vaccine as we think.
TA: So, ultimately, what’s your take on this?
Koci: For me, the right answer is to stay the course. Stick with what we know works. We need to be patient. We need to recognize we got ridiculously lucky with how quickly we were able to make a vaccine against this virus. There are a lot of diseases we’ve worked on for decades and still don’t have good vaccines for. And in this case, it’s not just one vaccine, it’s three – with more on the way – and in astonishing time. The fact we have these vaccines so quickly, and with high effectiveness has been the only bit of truly good news in all of 2020. Take the win.
We need to make enough mRNA to stretch to Proxima Centauri and back 3.75 times. This is going to be a big freaking deal.
But in all honesty, I don’t know if there even is a right answer to these questions. There are multiple ways we can go. They all come with tradeoffs. The direction we choose needs to be informed by science. But ultimately, the vaccination plan we choose has more to do with the values and priorities we have as a society. Who gets the vaccine first? Do we require vaccination for access to schools, work, travel, etc? How do we balance safety and speed? How much risk are we willing to accept in the race to protect the greatest number of people possible?
We all have a stake in this, so we all need to have say. Broad popular support for the path we pick is essential to the program’s success. But regardless of what the program eventually looks like, everyone needs to be clear that this is going to be a long, slow, complicated process. This will be the biggest logistical undertaking in our country’s history, maybe even human history. It’s bigger than landing humans on the moon. It’s bigger than D-day. When all is said and done, globally, it will be bigger than the pyramids and the Great Wall of China in terms of human accomplishments.
If that seems a ridiculous comparison think about this. The Pfizer-BioNTech vaccine requires two doses, each with 30 micrograms of mRNA. That’s 0.000001 ounces. It will take 470 kilograms of mRNA (1,036 pounds) to give everyone on earth both shots. If we were to line up all those strands of RNA end to end, they would stretch 296 trillion kilometers (184 trillion miles) or 31.29 light years. The star nearest to Earth (besides the Sun), Proxima Centauri, is only 4.2 light years away. We need to make enough mRNA to stretch to Proxima Centauri and back 3.75 times. (Credit @punkrockscience on Twitter for the idea for this comparison.) And on top of making astronomical amounts of vaccine, we have to go and physically find and inject everyone. Twice. So, this is going to be a big freaking deal.



