Study Shows Powered Prosthetic Ankles Can Restore a Wide Range of Functions for Amputees
For Immediate Release
A recent case study from North Carolina State University and the University of North Carolina at Chapel Hill demonstrates that, with training, neural control of a powered prosthetic ankle can restore a wide range of abilities, including standing on very challenging surfaces and squatting. The researchers are currently working with a larger group of study participants to see how broadly applicable the findings may be.
“This case study shows that it is possible to use these neural control technologies, in which devices respond to electrical signals from a patient’s muscles, to help patients using robotic prosthetic ankles move more naturally and intuitively,” says Helen Huang, corresponding author of the study. Huang is the Jackson Family Distinguished Professor in the Joint Department of Biomedical Engineering at NC State and UNC.
“This work demonstrates that these technologies can give patients the ability to do more than we previously thought possible,” says Aaron Fleming, first author of the study and a Ph.D. candidate in the joint biomedical engineering department.
Most of the existing research on robotic prosthetic ankles has focused solely on walking using autonomous control. Autonomous control, in this context, means that while the person wearing the prosthesis decides whether to walk or stand still, the fine movements involved in those movements happen automatically – rather than because of anything the wearer is doing.
Huang, Fleming and their collaborators wanted to know what would happen if an amputee, working with a physical therapist, trained with a neurally controlled powered prosthetic ankle on activities that are challenging with typical prostheses. Would it be possible for amputees to regain a fuller range of control in the many daily motions that people make with their ankles in addition to walking?
The powered prosthesis in this study reads electrical signals from two residual calf muscles. Those calf muscles are responsible for controlling ankle motion. The prosthetic technology uses a control paradigm developed by the researchers to convert electrical signals from those muscles into commands that control the movement of the prosthesis.
The researchers worked with a study participant who had lost one leg about halfway between the knee and the ankle. The participant was fitted with the powered prosthetic ankle and did an initial evaluation. The patient then had five training sessions with a physical therapist, each lasting about two hours, over the course of two-and-a-half weeks. After the training was completed, the participant did a second evaluation.
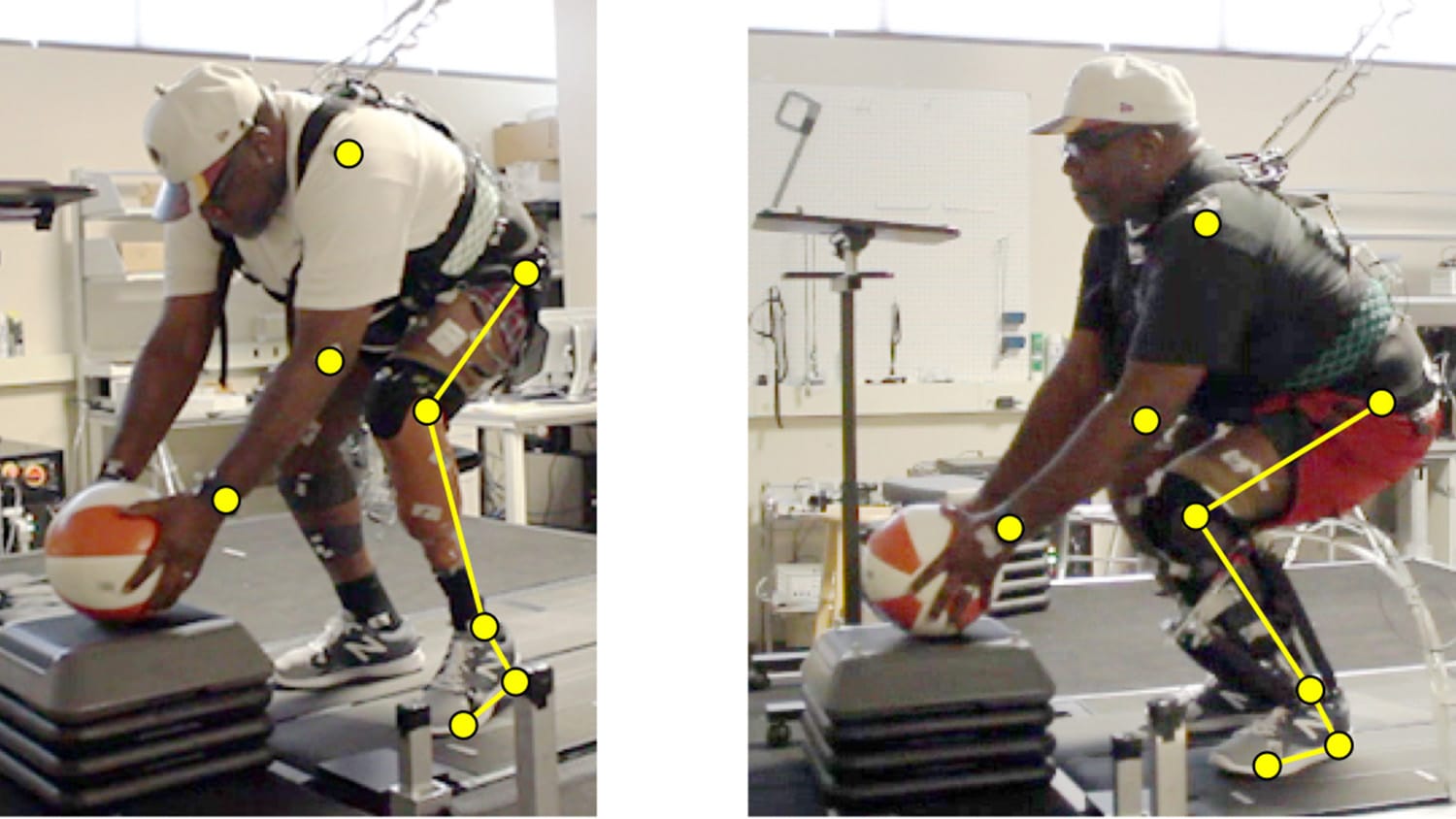
After training, the study participant was able to do a variety of tasks that had been difficult before, such as going from sitting to standing without any external assistance or squatting to pick something up off the ground without compensating for the movement with other body parts. But one of the most pronounced differences was the study participant’s stability, whether standing or moving. This was reflected in both empirical evaluations – such as testing the patient’s stability when standing on foam – and in the patient’s level of confidence in his own stability.
“The concept of mimicking natural control of the ankle is very straightforward,” Huang says. “But implementation of this concept is more complicated. It requires training people to use residual muscles to drive new prosthetic technologies. The results in this case study were dramatic. This is just one study, but it shows us what is feasible.”
“There is also a profound emotional impact when people use powered prosthetic devices that are controlled by reading the electrical signals that their bodies are making,” Fleming says. “It is much more similar to the way people move intuitively, and that can make a big difference in how people respond to using a prosthesis at all.”
The researchers are already having more people go through the training paradigm and are expanding their testing to assess the results of that training.
Before making this technology more widely available, the researchers also want to engage in real-world beta testing – with people using the robotic prosthesis during their daily routines.
“As with any prosthetic device for lower limbs, you have to make sure the device is consistent and reliable, so that it doesn’t fail when people are using it,” Huang says.
“Powered prostheses that exist now are very expensive and are not covered by insurance,” Fleming says. “So there are issues related to access to these technologies. By attempting to restore normal control of these type of activities, this technology stands to really improve quality of life and community participation for individuals with amputation. This would make these expensive devices more likely to be covered by insurance in the future if it means improving the overall health of the individual.”
The paper, “Direct Continuous EMG Control of a Powered Prosthetic Ankle for Improved Postural Control after Guided Physical Training: A Case Study,” appears in the journal Wearable Technologies. The paper was co-authored by Stephanie Huang, a graduate student in the joint biomedical engineering department; Elizabeth Buxton, in the Department of Rehabilitation Therapies at UNC Hospitals; and Frank Hodges of SunStone Lab LLC. The work was done with support from the National Institutes of Health under grants F31HD101285 and EB024570; and from the National Science Foundation under grant 1954587.
-shipman-
Note to Editors: The study abstract follows.
“Direct Continuous EMG Control of a Powered Prosthetic Ankle for Improved Postural Control after Guided Physical Training: A Case Study”
Authors: Aaron Fleming, Stephanie Huang and He (Helen) Huang, Joint Department of Biomedical Engineering at North Carolina State University and the University of North Carolina at Chapel Hill; Elizabeth Buxton, UNC Hospitals; and Frank Hodges, SunStone Lab LLC
Published: April 12, Wearable Technologies
DOI: 10.1017/wtc.2021.2
Abstract: Despite the promise of powered lower limb prostheses, existing controllers do not assist many daily activities that require continuous control of prosthetic joints according to human states and environments. The objective of this case study was to investigate the feasibility of direct, continuous electromyographic (dEMG) control of a powered ankle prosthesis, combined with physical therapist (PT)-guided training, for improved standing postural control in an individual with transtibial amputation. Specifically, EMG signals of the residual antagonistic muscles (i.e. lateral gastrocnemius and tibialis anterior) were used to proportionally drive pneumatical artificial muscles to move a prosthetic ankle. Clinically based activities were used in the training and evaluation protocol of the control paradigm. We quantified the EMG signals in the bilateral shank muscles as well as measures of postural control and stability. Compared to the participant’s daily passive prosthesis, the dEMG-controlled ankle, combined with the training, yielded improved clinical balance scores and reduced compensation from intact joints. Cross correlation coefficient of bilateral CoP excursions, a metric for quantifying standing postural control, increased to 0.83(±0.07) when using dEMG ankle control (passive device: 0.39(±0.29)). We observed synchronized activation of homologous muscles, rapid improvement in performance on the first day of the training for load transfer tasks, and further improvement in performance across training days (p=0.006). This case study showed the feasibility of this dEMG control paradigm of a powered prosthetic ankle to assist postural control. This study lays the foundation for future study to extend these results through the inclusion of more participants and activities.


