Vaccine Q&A: Vaccination Rates and New Mutations of the Virus
As the COVID-19 vaccination effort continues, there seem to be a lot of news stories about new mutations of the SARS-CoV-2 virus that causes the disease. This is raising a lot of new questions. How long might the vaccines protect us from COVID-19? What do the mutations mean? Is there any sort of relationship between the mutations and the vaccines?
To learn more, we spoke with Matt Koci, a virologist and immunologist whose work focuses on host-microbe interactions in birds. Koci is a professor in NC State’s Prestage Department of Poultry Science.
One clear takeaway message? If you are able to get vaccinated against COVID-19, you should.
This post is part of a series of Q&As in which NC State experts address questions about the vaccines on issues ranging from safety to manufacturing to how the vaccines will be distributed.
The Abstract: I’ve seen news stories about people who appear to have gotten infected with COVID-19 twice, and that this suggests that – at least for some people – immunity to the virus doesn’t last very long. Do we know how long immunity will last if we’re vaccinated? What are we doing to understand that? I’m guessing that the people who participated in clinical trials for the vaccines are being tracked, but what about everyone else who’s being vaccinated?
Matt Koci: I don’t know. At one point, I was under the impression that they were going to be tracking people getting vaccinated under the EUA [FDA’s Emergency Use Authorization] – and not just people who participated in the clinical trials. But the rollout has been so disorganized, and has varied so much from state to state, that I don’t think those plans would be operational anymore. But that doesn’t mean we won’t have data.
Knowing how long immunity lasts, knowing what aspects of the immune response are the most effective at providing protection, these are critically important things. We need to know this to know how best to use the vaccines and control the continued spread of COVID-19. We need to know this so we’ll know if we will need booster shots seasonally, annually or not at all. We need to know this to help inform how best to make the next generation of COVID-19 vaccines if it continues to mutate. Knowing this will also be really helpful in advancing our understanding of how to make vaccines for other diseases. So, a lot of people want to know the answers to these questions. I am certain that virologists, immunologists and physicians around the country (and beyond) will be collecting samples from all kinds of groups to make sure we understand the duration of immunity post vaccination.
TA: How quickly is SARS-CoV-2, the virus that causes COVID-19, mutating?
Koci: The good news here is that while fast mutation rates are typically a hallmark of RNA viruses, coronaviruses are the exception to that rule. They actually mutate very slowly compared to other RNA viruses. Looking at all the genomic sequences from all the SARS-CoV-2 isolates from around the world, on average there are just two nucleotide changes out of the 30,000 total nucleotides in its genome per month.
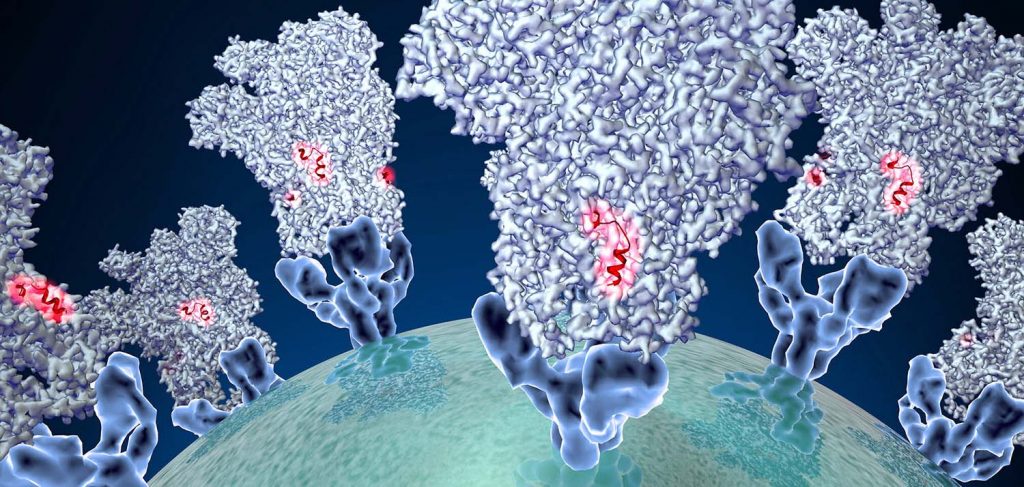
The other good news is that just because there are a few changes in the genome doesn’t mean the virus is really changing. A lot of those changes won’t affect how the virus spreads or how deadly it might be. In fact, it’s possible some mutations might make it less dangerous. But the concerning thing is that a few of the changes we see are in the spike protein. That’s the protein responsible for getting the virus into your cells, and it’s the major target for your immune system to make antibodies against. It’s also the part of the virus the vaccines are delivering to get your immune system primed and ready. Changes in the spike gene could lead to viruses that spread faster and/or viruses that can get around your immunity if you’ve already recovered, or if you’ve been vaccinated.
The news has exploded with reports of new variants. This is probably because countries around the world have increased how much they’re looking new variants, but it’s not the first time we’ve seen a new variant emerge. It feels like it was 10 years ago, but it was only in May of 2020 that there was a variant named D614G that seemed to spread faster than other strains of the virus and currently is the most common strain around the world.
Then, in December, we learned about the variant that is referred to as the U.K. variant, but is technically known as B.1.1.7 (scientists are great at naming things). This variant actually has 23 changes in its genome. Six of those changes don’t lead to changes in any of the virus proteins. However, the others do – and eight of those lead to changes in the spike protein. One of those spike protein changes, known as N501Y, appears to allow it to spread faster, more efficiently, than the current dominant circulating virus. The good news though is it doesn’t seem to be more deadly and it seems like the vaccine will still work against it.
However, more troubling variants have been reported in South Africa and Brazil that have a change in the spike protein known as E484K. This change makes the antibodies your immune system makes in response to the vaccine (or previous strains of the virus if you were infected and recovered) less effective. That doesn’t mean the vaccine won’t work, the T-cell part of your immune system may still be able to get the job done on its own. But it would be a lot better to have the one-two punch combination that both T-cells and B-cells bring to the fight. And what’s even worse is the variant from South Africa also has the N501Y mutation found in the U.K. variant – which means it can spread faster too.
How likely are there to be mutations that might mean bad things for us?
Then on top of those variants there are new reports of additional variants in California, but these are so new I don’t know if we know how those variants might behave differently.
So then the question becomes: How likely are there to be mutations that might mean bad things for us? We don’t know – but as we apply selection pressures to the virus, the likelihood of ‘bad’ mutations making it into the population goes up.
How does that work? Let’s use vaccination as an example. Getting vaccinated applies a selection pressure, because mutations that help a virus avoid detection by the vaccinated immune system will have an advantage over versions of the virus that don’t include that mutation. So, a virus that contains that mutation is more likely to reproduce and spread to other people. However, I want to be clear, this is NOT an argument against using vaccines. That would be like saying, “Thieves might figure out how to pick locks so there’s no reason to put a lock on my door.”
The vaccine is not causing this problem. Instead, think of it as a race between getting enough people immunity before the virus has a chance to mutate. Every infected person is one more chance for the virus to mutate, increasing the chances that a new variant emerges that spreads faster, makes people sicker, or can get around immunity. This is one reason why it is critically important for people to wear masks, wash hands, maintain social distance, and do everything they can to slow the spread of COVID-19.
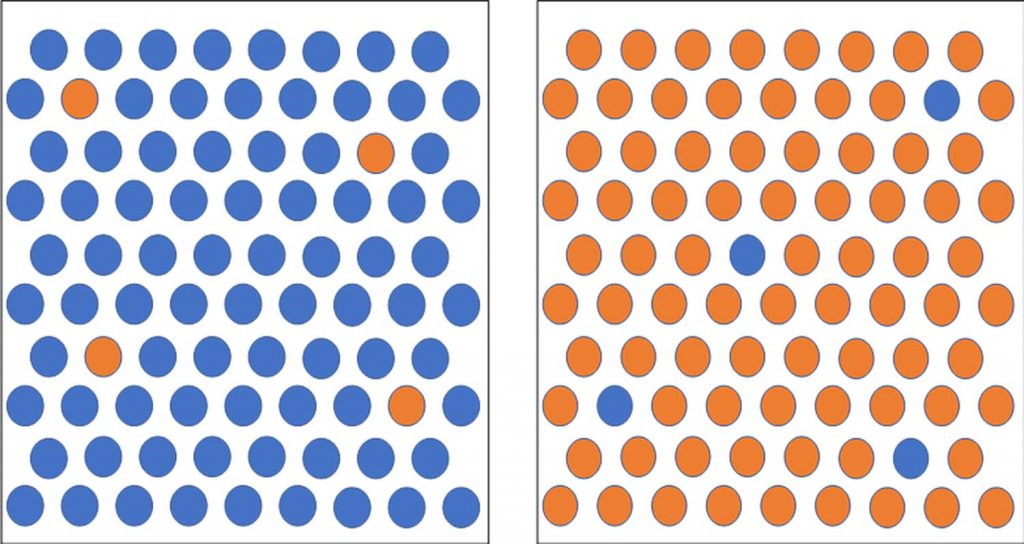
Think about it like this [see image above]. Each blue dot is someone who’s been vaccinated. Each orange dot is someone infected with SARS-CoV-2. If almost everyone is immune and just a few people are sick, there are only a few people coughing virus out. And given the slow mutation rate, the odds that one of those people cough out a virus that defeats the immunity of the population is low. However, if you have the opposite – lots of infected people coughing out virus and just a few people with immunity – the odds of a problematic mutation making its way into the population is greater. Again: this is why it is so important for everyone to keep social distancing and keep wearing masks until we reach herd immunity. [Editor’s note: Herd immunity is when enough people in a population are immune to a disease that the virus or bacteria that causes that disease can’t spread, providing protection to others in the population who don’t have immunity.]
TA: I asked about mutations because, in our last vaccine interview, you said that you think we need to be vaccinating between 0.5% and 1% of the population each day. I was wondering where that estimate came from.
Koci: The number of 0.5-1% wasn’t based directly on the virus’s mutation rate, obviously – there’s no way of knowing exactly how long it might take for a mutation like that to happen. It was really my attempt to come up with a range that I thought was achievable, expressed a real sense of urgency, and would ensure we catch up to and quickly pass the number of people infected with COVID-19 to achieve herd immunity* as quickly as possible. For herd immunity we don’t need everyone to be immune, but we don’t know exactly what we need. I’m a big advocate of going for as many as we can get. If we shoot for just enough and miss, we’re in trouble. If we shoot for everyone and miss, we should still be well above the minimum necessary. So, with that in mind, and to keep things simple, I used the whole U.S. population as a reference (331 million) that people can scale down from as needed.
[*Editor’s note: There is strong evidence the vaccines prevent severe symptoms of COVID-19, but we do not yet know if the vaccines prevent you from being asymptomatically infected. This means that someone who has taken the vaccine may still be able to transmit the disease to others. Masks, social distancing and handwashing are still encouraged, regardless of whether you’ve been vaccinated. You can learn more here about the possibility that vaccinated people may still be able to transmit COVID-19. This is an ongoing area of research, and we will share new information when it becomes available.]
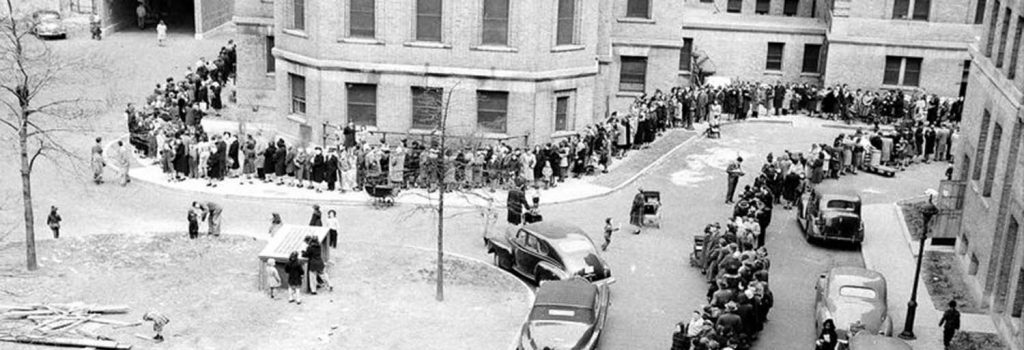
Why I think it’s achievable: In 1947 there was a reintroduction of smallpox in Manhattan. They vaccinated roughly 6 million people in New York City in about a month. In 1947 the population of NYC was around 7.8 million. Reports are that they vaccinated 5 million people in about two weeks. That’s about 5% of the population per day. (As a quick aside, I will note that one reference disputes those numbers and suggests the rate was closer 1%). Smallpox has a reproductive rate, or R0*, between 3 and 6, which is similar to what COVID-19 would be without the 3 Ws. That means smallpox spreads at about the same rate at COVID-19, so vaccination rates that were successful at containing smallpox is a good place to start for containing COVID-19. [*Editor’s note: reproductive rate is the average number of people who would be infected by a virus from a single case. It is used as a way of estimating how quickly a disease will spread through a population.]
The NYC smallpox example shows us that, from a logistics standpoint, we can set up systems to vaccinate a lot of people in a hurry when we recognize the threat and take it seriously. The issue today is: Do we have the vaccine supply to do those kinds of numbers?
If we vaccinated 5% of the U.S. population per day, that would mean vaccinating 16.6 million people per day. You can do 5% (if it really was 5%) when it’s just a small region of the country. But when it’s the whole country, and the rest of the world needs vaccines too, and everyone needs two shots, 5% is probably unrealistic.
But 1% per day could be possible. Logistically, that’s not far off from how many COVID tests we’ve been doing per day in N.C. Over the past month or so, we’ve been doing around 70,000 tests per day. That’s roughly 0.7% of N.C.’s population every day. The bottleneck on tests is the PCR work in the lab, not swabbing people. The 15-minute monitoring period post-vaccine poses some logistical challenges, but there’s no reason why we can’t do at least as many vaccinations as we do tests plus a little more (say 105,000) and call it 1% per day: just replicate drive-through testing, but for vaccines.
We need to get creative. Set up centralized centers as accessible to as many people as possible.
Some will say the need to keep the mRNA vaccines super-cold is the issue that will keep us from being able to vaccinate that many people. They’ll say the testing centers don’t need all those super cold freezers, so this is different. I disagree. The cold chain certainly complicates things, but it is solvable. Plus, hopefully, the Ox/AZ vaccine will be approved soon. There are 100 million doses ready to go in the U.S. as soon as it is. That vaccine doesn’t have to be kept as cold, so shipping and storage is easier. With a centralized plan, you could distribute vaccine based on proximity to freezers and dry ice. We need to get creative. Set up centralized centers as accessible to as many people as possible. Use voting precincts. Use Wal-Marts. Local high schools. Amazon purchased a bazillion freezers, they’ve partnered with cryogenic freight companies to optimize their delivery process; they’re ready to be part of the solution.
Let’s put it this way: the vaccine isn’t laundry detergent, but Amazon has built a system to match my order to the nearest fulfillment center to ensure that my detergent gets to me as fast as possible. Why are we trying to reinvent the wheel here?
The sense of urgency: People are clearly tired of doing what needs to be done to slow the spread of COVID. That means people are being less vigilant and taking more risks. I get it. I’m burned out on COVID-19 too. I want to see friends and family. But cases keep going up. There is little to no sign they will slow until we cross the 50% infected threshold and the virus starts running out of people to infect. All this rampant spread means we have this ever-increasing number of infected people. Each one is another ticket in the virus mutation lottery. And now we’re starting to enter a period where the virus is going to start coming under selection pressure from the small but growing population that has some immunity.

There have been more than 24 million confirmed cases in the U.S., and that number is currently growing by 200K per day. Most of those who have recovered likely have some immunity. There is a small but growing number of people who are being treated for COVID-19 with monoclonal antibodies like the therapy President Trump received. People are still being treated with convalescent plasma. And we have a growing number of people who have been vaccinated. All these people, while still a relatively small percentage of people in the U.S., present immune selection pressure on the spike protein to mutate – meaning they increase the likelihood that vaccines will become less effective.
I want to make this absolutely clear: the vaccines are necessary.
In the lab, if I want to generate a viral mutant that is resistant to antibodies, I expose high levels of virus to low levels of antibodies. And right now, it seems like those are the conditions we have at the population level. Which is scary. If you have the opposite mix, 10-100 times more antibodies than virus, it’s a lot harder for mutants to pop up. To be clear, a culture plate in a laboratory isn’t the same thing as a human out in the wild, but basic principles are the same. If you can get everyone immunity faster than the virus can mutate around the vaccine you stop the spread. That’s one of the reasons why you don’t get herd immunity without vaccines.
And again, I want to make this absolutely clear: the vaccines are necessary. Vaccines can play a role in dictating which virus mutations are most likely to thrive, but the virus is going to mutate anyway. The faster we get everyone immunized, the less chance the virus has to mutate.
At any rate, the big idea is that if we can get 1% of the population vaccinated per day, that gets everyone vaccinated in roughly 130 days. Assuming an aggressive vaccination program wouldn’t kick-in until around mid-February, we’re looking at June or July. If the vaccination rate is 0.5% per day, takes things out to about 230 days, or September/October. Those are the date ranges people have been promised. Those are the date ranges we need to be shooting for. If we’re not close to done by then, forget about people continuing to do the right thing.
With three companies making vaccine it would be tight, but I think supplying enough vaccine to get everyone their first shot at 1% per day is doable. That second shot is probably where the supply chain falls short, but that doesn’t mean we shouldn’t shoot for it. Get as close to 1% vaccinated for 21 days (when boosters start coming due) then drop off to 0.5% per day and ramp back up to 1% as additional vaccines are authorized for emergency use.
TA: What vaccination rate is needed in other parts of the world?
Koci: I don’t know. There’s no way to know when viral evolution will spit out a “winning” number that makes the virus even more problematic or increases its immunity to vaccination. That’s why I call it Satan’s Lottery. But the more time it takes to vaccinate the population, and the more pressure we apply to the virus, the greater the odds that we see a resistant strain of the virus. Ideally, once we get a program working in the U.S., E.U., and Asia, and we’ve gotten past some critical tipping point (50-60%) immunized, we need to see the developed countries start devoting resources to try and stamp this out like smallpox and polio. We’ll want to get to work on it as fast as possible. Vaccinating 1% of the population a day for the rest of the world is almost certainly not possible, but if it were as low as 1 million per day for all of Africa it would take more than three years.
TA: How much genomic testing should the U.S. be doing to track mutations?
Koci: The short answer is: a lot more than we’re doing. As of last December, we were sequencing 0.3% of the identified cases. That ranked us 43rd in the world. The U.K., which has been sequencing around 7% of the viruses it finds in people, was ranked 8th. I hope, I assume, we’re doing better than 0.3% now, but how much better I don’t know. What percentages of the positive cases should we be sequencing? I don’t know what that number should be.
As a scientist I always want more data, but with so many new daily infections, it becomes hard to take resources away from testing. Still, I would think sequencing 2-5% per day would be smart. It would also be nice if we could store an additional 5-10% to go back and sequence later if we end up finding something worrisome and need to take a closer look at how much it might really be out there. But with so many cases and freezer space at a premium right now I can understand why that might not be possible, but one lesson we should have learned from last February and then again from last December, the first case you find is NEVER the first case. So, by the time you find something, it’s already out there, especially if you aren’t really looking that hard to start with.


